WELCOME! This website is designed to help Hispanic children and their families better understand and manage Atopic Dermatitis (or what some refer to as "Eczema"). The site is not overly detailed but is instead meant to provide general information and practical treatment insights. It is used to support your Dermatologist.
Atopic Dermatitis is a common skin disorder that affects all ages but ESPECIALLY children. There is a lot of valuable information available about Atopic Dermatitis, but there are also many misconceptions.
Please Note:
- This site is completely FREE.
- There are two versions of this site, one in Espanol and one in English.
- If you were directed to this site by your Dermatologist (a doctor professionally trained in the care of skin). First and foremost, always trust the information and follow the treatment instructions exactly as provided by your Dermatologist.
Atopic Dermatitis (Overview)
- affects 8-15% of the childhood population in the U.S. and is quite prevalent in Hispanic people. It can start in newborns but usually begins between the ages of 1 and 5.
- is chronic and is NOT “curable” in an instant, but most patients improve dramatically as they get older. It disappears entirely in some patients, usually before age 20.
- is NOT contagious
- is caused mainly from genetic qualities in a person that is outside of his/her control. A person’s immune system seems to over respond in patients with Atopic Dermatitis.
- is sometimes made worse by environmental factors such as fragrances, pet dander, temperature changes, fresh cut grass, wool, and many others.
- is especially problematic due to itching. Other symptoms including red scaly skin patches, thickening and dryness of the skin and sometimes swelling.
- is prone to “flare-up” for often unknown reasons.
- is almost never controlled with changes ONLY in diet, lifestyle, and supplements.
- is usually mild and aggravating but can be very serious and life changing as well.
- is often associated with other disorders such as asthma and hay fever.
- is best managed with the help of a Dermatologist
General Treatment Strategies For Atopic Dermatitis
(1) You should use mild, unscented soaps. Plain White Dove is outstanding, and other good brands include Cetaphil, Aveeno, CeraVe and Neutrogena, though this list is not exclusive. Fragrances of all types MUST BE AVOIDED in all cleansing products.
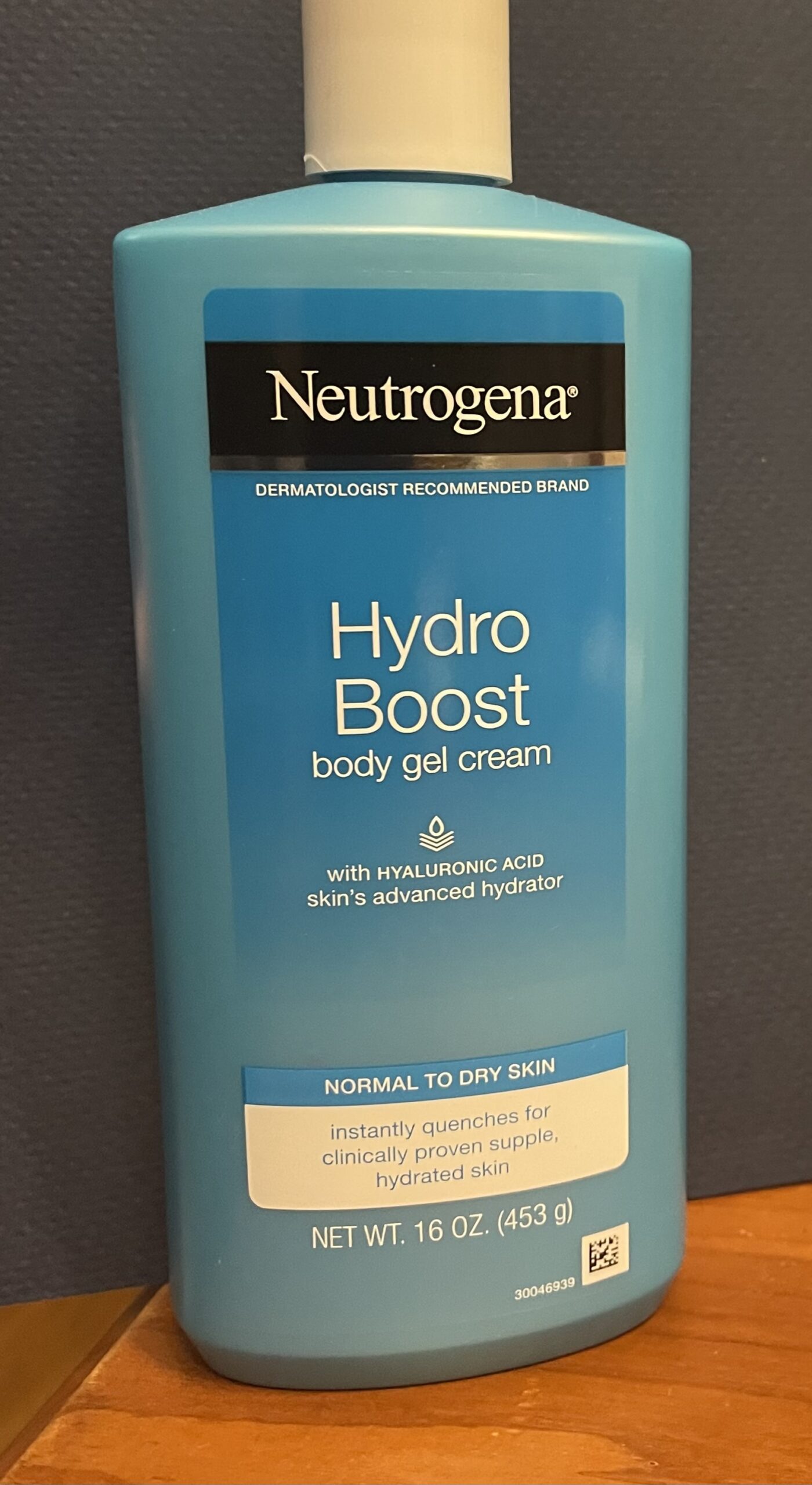
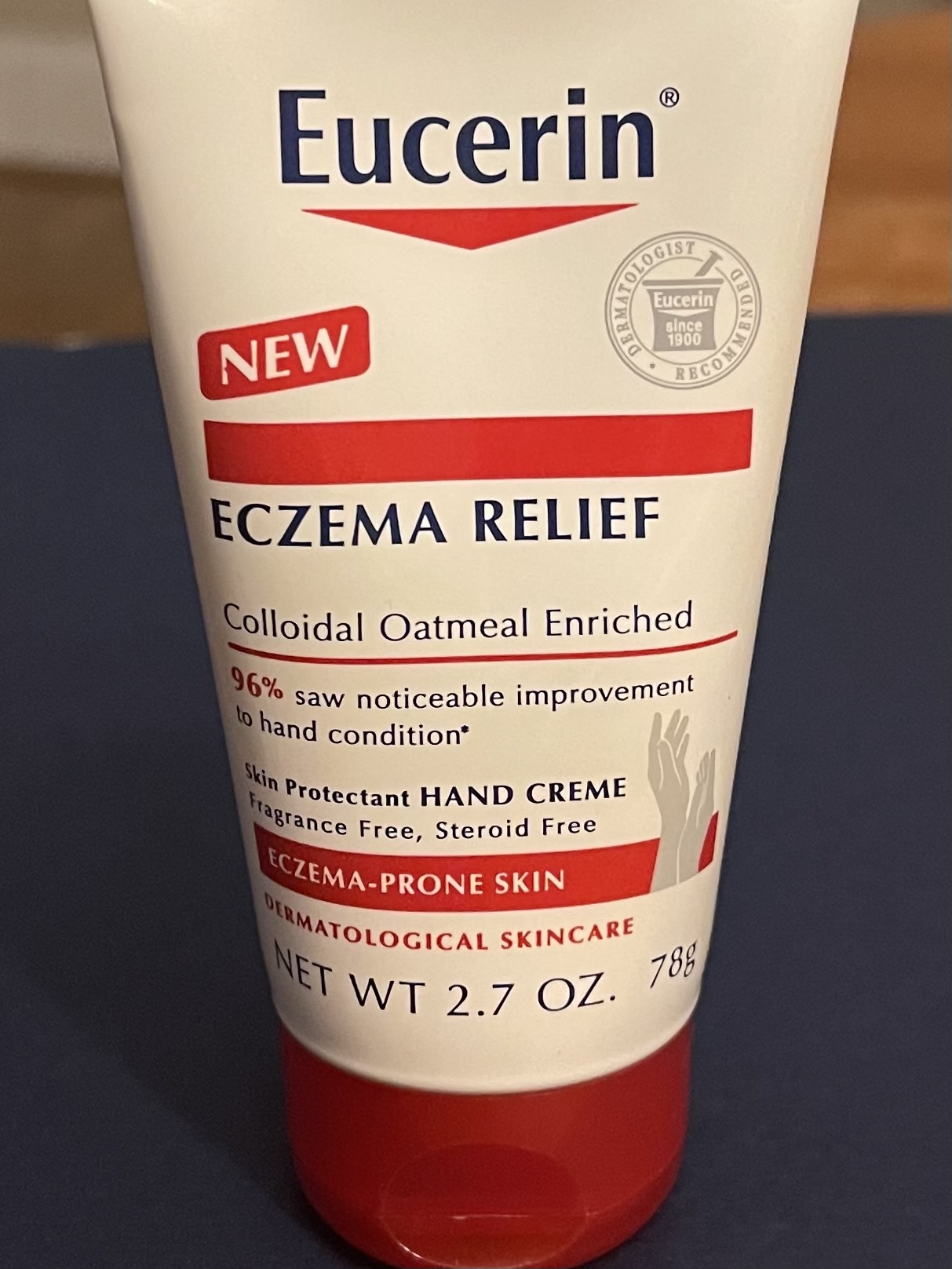
(2) It is very important to consistently keep your skin moisturized with a fragrance-free moisturizer. You should moisturize your skin even when the dermatitis is under good control because this can help control the frequency and severity of the rash and the itching. There are some outstanding moisturizers on the market including products by Cetaphil, Aveeno, Neutrogena, Eucerin, CeraVe, Curel and others. Bear in mind that cost is a big factor in choosing a moisturizer. If you are on a tight budget, plain Vaseline petroleum jelly is inexpensive but extremely good – it is more greasy but very effective.
(3) There are certain exposures that may make your skin worsen or flare-up. These include sudden temperature changes, wool, pet dander, dust and dust mite, some pollens, freshly cut grass and fabric softeners. Products of any type containing FRAGRANCES should be avoided. This includes body sprays, colognes, perfumes, and any number of related products. The bottom line is that it is a good idea to use wise judgment in terms of what you expose your skin to in the environment. But remember that no matter how cautious you are, if you have Atopic Dermatitis, you will have flare-ups.
(4) Find a Dermatologist and trust that doctor in the care of your skin. Your Atopic Dermatitis can change, and you will need your Dermatologist to help you navigate your Atopic Dermatitis over time.
Medications
(1) Topical Steroids are used for treatment, depending upon the severity of the patient’s disease. Topical steroids help decrease skin inflammation and itching. They range in potency from weak to extremely strong. The potential for side effects with these products is low, provided they are used appropriately. For this reason, it is important to follow carefully the instructions given to you by your Dermatologist. For instance, some areas of the body such as the face, underarms, and groin area, will not tolerate strong topical steroids because these areas are sensitive and more prone to developing side effects (such as thinning of the skin). But for the most part, topical steroids are safe and very useful for Atopic Dermatitis. One other important piece of info regarding topical steroids is that your skin can develop tolerance (i.e. it “gets smart to the steroid”) if the medication is used for an extended period and continuously. Therefore, when your dermatitis is well controlled, do not continue using the topical steroid regularly. Instead, taper down with less frequent applications, and if possible, try to stop using the topical steroid for a while. In this way, you can “keep ahead” of your dermatitis, and the medication will show continued usefulness over a longer period. There are many types of topical steroids, and they come in various vehicles (e.g. ointment, foam, cream, gel etc.). Your Dermatologist will choose the one(s) that will work best for your situation. Many products are in generic form and are inexpensive whereas others are more expensive. Here are a few examples:
Super Potent: Halobetasol propionate, Clobetasol Propionate
Strong: Fluocinonide, Halcinonide
Medium: Triamcinalone, Mometasone
Mild: Desonide, Hydrocortisone
(2) Antihistamines can be utilized for itch control. Your Dermatologist might employ these safe and effective medications. The best ones do not cause excessive sleepiness, and these include Allegra (Fexofenadine), Claritin (Loratadine), Zyrtec (Cetirizine) and Xyzal (Levocetirizine). Others such as Benadryl (Diphenhydramine) can be helpful but tend to cause more drowsiness.
(3) Antibiotics are sometimes prescribed if the skin is heavily affected as bacteria tend to colonize areas of dermatitis. Decreasing those bacteria counts can help the dermatitis.
(4) Other non-steroid containing topical products are also available and may be prescribed. Examples include Eucrisa (Crisaborole), Elidel (Pimecrolimus), Protopic (Tacrolimus) and Opzelura (Ruxolitinib). They tend to be safe and can be used more frequently. They can be expensive.
(5) Steroids (such as Prednisone and Prednisolone) might be necessary from time to time, especially for patients going through particularly bad flare ups of Atopic Dermatitis. Steroids are good for short bursts but are not used for long term treatment.
(6) Stronger Medications that are taken by mouth or injection (known as “systemic treatments”) are sometimes extremely useful and life-changing for patients that have more severe Atopic Dermatitis. These are typically utilized when other treatments have failed. Examples include Dupixent (Dupilumab), Adbry (Tralokinumab), Rinvoq,(Upadacitinib), Methotrexate, Azathioprine and Cyclosporine. Your Dermatologist can help you decide if any of these medications are necessary for you.
Do Not Be Discouraged
A reliable treatment plan can be determined for every patient. Your Dermatologist is well equipped to help you tackle your Atopic Dermatitis. It may take a while to find the perfect treatment strategy for you – be patient! There is most definitely hope, and help is on the way!
Photographic Examples of Atopic Dermatitis
Hands and fingers are commonly affected.

Even babies can be severely affected.

Bumps and thick scales are frequent.

The bends of the elbows and knees are commonly affected.

Severe cases can cover much of the body.

Examples of Products Available Without a Prescription That Might Be Considered for Daily Management of Atopic Dermatitis
Neutrogena products are outstanding.
Non-fragrance body washes can be helpful for bathing.

Eucrin products are mild and fragrance-free.
Mild, non-fragrance containing soaps are important.

Frequent moisturizing is important. Here are 3 examples of many that are on the market and can be bought without a prescription.
